Below is an article written by Ron Leavitt, AUD which was published in American Academy of Audiology as part of their March/April 2025, volume 37, number 2, Audiology Today issue. Clicking the link below will download Ron’s article.
Ron Leavitt featured on the informative podcast “Listen Up”
Recently Dr. Ron Leavitt was on “Listen Up” an informative podcast by the Arizona Hearing Center and hosted by Mark J Syms, MD. The podcast seeks to educate the public on the necessity of taking care of one’s hearing. Below is a link to the podcast video:
Dr. Ron Leavitt – Hearing Health and Comprehensive Auditory Rehabilitation
Recently Dr. Ron Leavitt was on “Listen Up” an informative podcast by the Arizona Hearing Center and hosted by Mark J Syms, MD. The podcast seeks to educate the public on the necessity of taking care of one’s hearing. Below is a link to the podcast video:
Pathways Interview with Dr Ron Leavitt
Below is a link were Dr. Ron Leavitt was interviewed by Dr. Frank Musiek about both his early career and the current state of hearing aids
Pathways Interview with Ron Leavitt, Director, Corvallis Hearing Center, Corvallis, Oregon
Hearing Loss Hearing Aids and Brain Health
Below is a recording of Dr. Leavitt and his clinicians giving a speech on the importance of proper hearing aid fitting and brain health:
American Academy of Audiology Conference 2023
 Dr. Ron Leavitt and his assistants Holly and Andrea at the American Academy of Audiology Conference 2023
Dr. Ron Leavitt and his assistants Holly and Andrea at the American Academy of Audiology Conference 2023
Hearing Difficulty?
Hearing Difficulty?
It’s Important to Know the Business You Are In
Dr. Ron Leavitt, Audiologist
A noted entrepreneur once said “It is important to know what business you are actually in.” In recent years this quote has taken on new meaning for hearing health care providers.
In the past some audiologists may have thought we were in the hearing aid sales business. Then cochlear implants came along and that view was broadened to include a more encompassing term such as the “hearing improvement business” since hearing aids were no longer the only tool in the toolbox.
Today hearing health care providers are faced with a mountain of data suggesting we are in the cognitive optimization business.
Specifically, it is now known that when hearing loss is untreated or improperly treated, a host of anatomical and physiological changes occur in the brain that result in a phenomenon known as “synaptic pruning and resource reallocation.”
While synaptic pruning is used by the healthy brain to minimize those pathways that are nonessential to existence, when hearing loss is improperly treated synaptic pruning and reorganization takes place in critical areas of the brain associated with higher order reasoning. Such unfavorable reorganization/pruning may be a gateway to dementia whose strong relationship to hearing loss has been well documented.
The obvious question then becomes what should we be doing to prevent such an outcome? First, when friends, family or colleagues start saying you are having hearing problems act immediately to get a comprehensive hearing test. There is likely a point of no return where the brain is too improperly pruned/reallocated to recover (see https://corvallishearing.com/1feb2021 for more in-depth discussion).
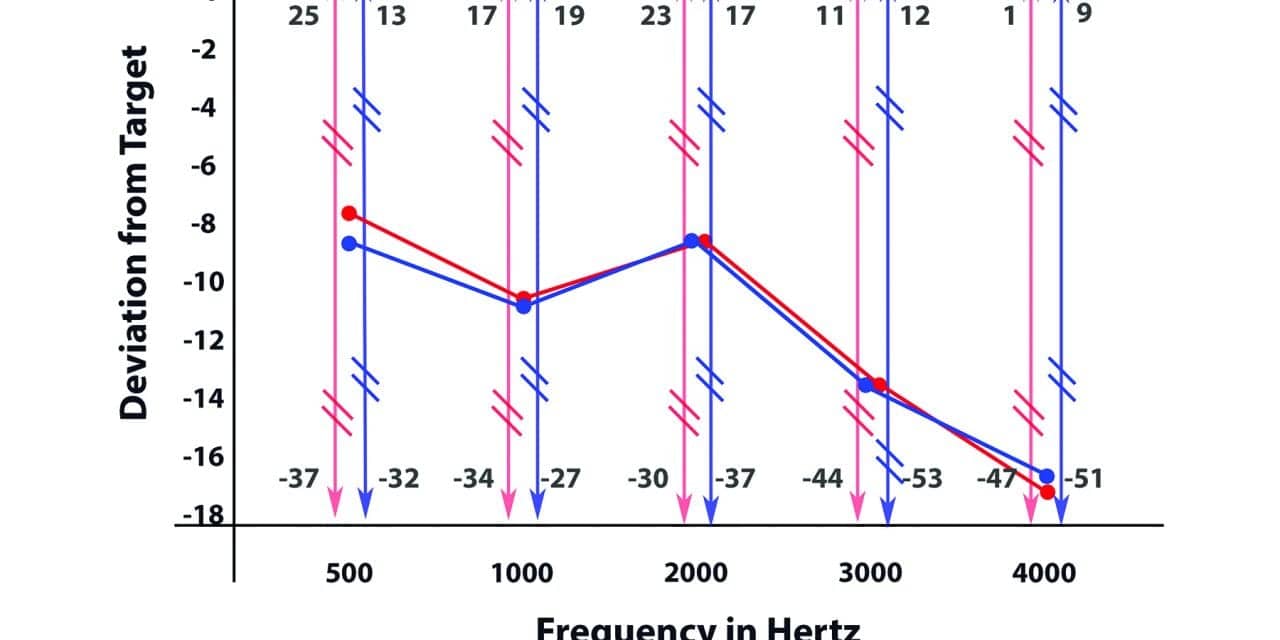
Next, every hearing aid and cochlear implant must be programmed so as to provide audibility of the greatest number of speech sounds possible within the limitations of the individual’s hearing loss. Unfortunately, such programming rarely occurs (see https://corvallishearing.com/2feb2021 or https://corvallishearing.com/3feb2021 or https://corvallishearing.com/4feb2021 for more in depth explanation).
Next, you must work to maintain optimized hearing of speech sounds. Such maintenance entails annual hearing and hearing aid/cochlear implant checkups. Hearing rarely gets better over time and some causes of hearing loss result in a fairly rapid degradation of hearing in a relatively short time frame. As such, hearing aid reprogramming may be necessary on an annual basis or sooner.
Additionally, hearing aid and cochlear implant performance may degrade over time, particularly when used in high humidity or dusty/polluted environments or worn with excessive amounts of hair spray.
Finally, we must all take some initiative to stay physically active and eat well as contemporary research has shown both are critical areas of intervention in cognitive optimization for both children and adults (see https://corvallishearing.com/5feb2021 and https://corvallishearing.com/6feb2021 and https://corvallishearing.com/7feb2021 and https://corvallishearing.com/8feb2021 for more info).
For anyone interested in more information on this topic we will be presenting this information at our next “virtual” Better Listening Seminar and on our website in the near future. For more info call (541) 754-1377.
Hearing Loss and the Brain
Frequent readers of this section are well aware that hearing loss changes the brain in ways that foster dementia. Those who have missed this news are referred to the following article (https://corvallishearing.com/hldementia)
Unfortunately, recent information suggests that well before dementia sets in there are a large series of changes that take place that make the brain function in abnormal ways (https://corvallishearing.com/congenital-deafness).
These new findings use radiographic techniques to show the numerous essential inter connections that exist between the primary and secondary auditory areas of the brain and all other parts.
These brain interconnections must be functional for people to completely comprehend spoken or written language or even maintain appropriate social behavior. To quote Dr. Kral and his colleagues, “The experienced adult brain relies on higher-order representations for generating expectations about the environment based on the context and behavioral goals. These expectations are possible since the brain has developed a meaningful representation of the world (sensory information) that is constantly updated and compared with external events. With the mature micro circuitry the auditory (area of the brain) can integrate bottom-up and top-down (sensory and intellectual) information flow. In cases of conflict between the input (from the senses) and these (memory) expectations, error signals drive plastic changes and learning. These processes require experience and a functional interareal (whole brain) and intrinsic (brain) circuitry.”
Stated differently, looking only at the auditory area of the brain is missing the point.
Knowledge of the critical importance of these inter connections brings us to an obvious question: What should we be doing to foster interconnected brain health?
Fortunately, we have research that addresses this intervention question.
First, there must be a foundation that allows for hearing the maximum number of speech sounds in individuals with hearing loss (https://corvallishearing.com/audibility).
Depending on the level of hearing loss, this first rule mandates use of hearing aids or cochlear implants long before hearing loss becomes chronic. Again quoting Dr. Kral and colleagues, “changes (due to hearing loss) in columnar microcircuits (deep and superficial brain connections) and interareal couplings (connections within the larger parts of the brain) limit the outcome of sensory restoration (hearing aids and/or cochlear implants) if performed late in life.
Stated differently, there is a point of no return. The body is a habitual machine and if you let it develop bad physiological habits (untreated hearing loss) for a long period of time, these bad habits cannot be undone.
However simply obtaining timely hearing aids or cochlear implants is not enough. These devices must be properly programmed and most are not (https://corvallishearing.com/oregon-fitting-errors)
Secondly as noted by Kral and colleagues, the individual must maintain brain stimulating, language-rich social contacts. (Use it or lose it).
To summarize, a healthy brain requires maximum audibility of speech sounds and intellectually stimulating use of those audible words.
For more in-depth discussion of this issue the reader is referred to the following summary (https://corvallishearing.com/entrain-brain).
Hearing Aids for People with Normal Hearing?
Much research has focused on patients who self-report listening difficulties, but show normal results on the typical pure tone hearing test where you raise your hand, push a button or say “yes” when you hear the tone.
In fact, it is estimated some 26 million people in the U.S. self-report listening difficulties with normal pure tone results (see https://corvallishearing.com/hearing-difficulties for references ).
This 26 million figure would account for nearly 70% of the 37.5 million people in the U.S. who have suspected listening difficulties per the National Institutes of Health estimate.
The literature notes there are a number of auditory disorders that may not produce hearing loss as measured by pure tone testing. These disorders include Central Auditory Processing Deficit, Auditory Neuropathy Spectrum Disorder, Cochlear Synaptosis, Hyperacusis and tinnitus to name a few.
It is not surprising then that pure tone testing popularized in the early 1940s does not address these more recently-identified auditory maladies.
In a previous article we noted several other tests are often more diagnostically revealing for the disorders listed above. However, the question for most patients so afflicted with any of these disorders is “What can be done to treat it.”
Unfortunately, the treatment of these disorders is less clear cut than the diagnostic tests used to identify them.
In a recent article Humes (2020) made the case for use of hearing aids with many such patients who show normal pure tone test results (see https://corvallishearing.com/normal-hearing).
In the case of tinnitus (the perception of ringing, buzzing, whooshing sound or music when no sound is actually present) the hearing aid recommendation is often supported. Research has shown oftentimes the brain is essentially turning up the volume looking for sounds that are no longer as loud as they once were before the individual experienced tinnitus. Thus, hearing aids can amplify these slightly less loud sounds back to their original volume and the perception of tinnitus in as many as 60% of patients is improved.
In the case of Hyperacusis (heightened sensitivity to sound, with aversive or pained reactions to normally-loud environmental sounds) this disorder is thought to result from the brain’s loudness mediating function being set at too low a volume. As such one recommended treatment is gradual introduction of more sound oftentimes from a very low-volume hearing aid combined with counseling to calm an apprehensive patient who is already concerned about too much sound. (see https://corvallishearing.com/tinnitus for discussion).
By contrast in 260 patients with Auditory Neuropathy Spectrum Disorder, 61% of patients reported little or no hearing aid benefit (see https://corvallishearing.com/auditory-neuropathy).
In short, successful use of hearing aids among patients self-reporting listening difficulties with normal pure tone results depends heavily on the correct diagnosis. To quote Ghandi “A correct diagnosis is three-fourths the remedy.” It is then imperative that in-depth testing beyond the conventional pure tone examination be completed before any hearing aid recommendation is made for such patients.
American Academy of Audiology 2020 Presentation
The international American Academy of Audiology conference for 2020 was cancelled due to COVID-19. However, they invited us to do a 90 second video on our scheduled presentation. This is our video of our session.
November 2019 Seminar
Brain Resource Preservation & Hearing Aids
This week Ron Leavitt, Au.D and Carol Flexer, Ph.D are presenting our research findings at the International Conference of the American Speech Language and Hearing Association in Orlando, Florida.
Hearing Loss and Falls
Falls are pervasive among people over age 65 in this country. Making this problem worse, the incidence of falls among people with hearing loss are three times greater than those with normal hearing when other risk factors are equated.
The Center for Disease Control reports that every second an older person in this country falls, making falls the number one cause of accidental injury and death in people over age 65.
In 2014 alone, older Americans experienced 29 million falls causing seven million injuries and costing an estimated $31 billion in annual Medicare costs, according to a new report published by the Centers for Disease Control.
In addition, falls are the number one cause of traumatic brain injury in this country affecting 5.3 million who routinely suffer cognitive and physical impairments for months or years after the injury. Further, traumatic brain injury has been positively associated with epilepsy, Parkinson’s and Alzheimer’s disease which often signal an end of an individual’s independence.
In an attempt to stem the tide of frequent falls in the elderly the Mayo Clinic group has offered the following advice:
- Discuss any fall you have with your doctor and have your medications checked for those which may be contributing to poor balance.
- Engage in physical activity such as walking to strengthen your legs and improve your balance.
- Wear sensible shoes to maintain better balance. High heels and socking feet are not recommended.
- Remove tripping hazards from the house such as loose rugs, loose wiring, phone cords, extension cords, immediately cleanup all water and oil spills when they occur and use rubber mats in the bathtub/shower with grab bars.
- Light up your living space with night lights in all walkways and a lamp near your bed. Use high illumination bulbs all over the house.
- Use handrails on both sides of all stairways and use nonslip surface on all wooden stairs. Occupational therapist can assist you in making your house fall proof.
In addition to these recommendations noted above, we are highlighting important strategies for fall prevention that go beyond those provided by the Mayo Clinic group. Join us at 2:30 to 4 PM on November 14th at Corvallis Good Samaritan Hospital Conference Room B where we will be offering a fall prevention workshop. The public is invited. No personal information will be taken, and free refreshments will be served.
At this November 14th meeting active people in their 70s, 80s and 90s will be discussing the strategies they have used to remain physically active, free of frailty and free of falls for years. In addition, our new book on Lifetime Physical Fitness will be made available to workshop participants for a nominal fee as frailty is highly associated with falls in contemporary research.
If you or a loved one are at risk for falls this conference is for you. For further information, contact Corvallis Hearing Center at 541- 754-1377.
Hearing Loss and the Brain: A Story of Evolution
At times, medical knowledge moves forward in leaps and bounds. At other times such knowledge moves forward in a more gradual fashion. Such has been the case with our knowledge of the effects of hearing loss on the brain.
Seven years ago, Dr. Frank Lin of Johns Hopkins Medical University reported that hearing loss was highly associated with dementia and accelerated brain shrinkage. At that time, our medical knowledge on this topic took a giant step forward.
Since that report, our understanding of this relationship has been more evolutionary. For example, Drs. Glick and Sharma showed that untreated and poorly treated hearing loss results in a scrambling of brain resources.
These researchers showed improperly treated hearing loss results in inappropriate use of the frontal and prefrontal areas of the brain. Typically, these two areas of the brain are associated with memory and reasoning. However, in the case of poorly treated hearing loss, these two brain areas are used for understanding speech, lending credence to Dr. Lin’s hypothesis that hearing loss may overwork the memory and reasoning areas of the brain.
On a positive note, Glick and Sharma showed that properly fit hearing aids may reset the brain so that the auditory area is once again used for listening. Now the frontal and prefrontal brain areas can resume their normal functions.
More recently, it was discovered that hearing loss upsets the normal rhythmic pulses and interconnections the brain uses to communicate among its different functional areas.
Within the last few months, two separate reports out of Boston and Northwestern Universities showed reestablishing appropriate pulse rates among these different areas of the brain results in significant memory improvements in older people.
These studies, when considered together, suggest the possibility that properly treated hearing loss with hearing aids, perhaps combined with brain pulse resetting, may combat the devastating effects hearing loss may have on memory.
Currently, several large-scale studies are under way, examining the potential therapeutic benefit of properly fit hearing aids and brain pulse resetting on memory. In the interim, it appears medically prudent to treat hearing loss sooner rather than later, as the average delay between diagnosis of hearing loss and treatment has recently been reported to be nine years. It is no longer appropriate to view hearing loss as an inconvenience that can be ignored.
At our clinic, we are currently reviewing the records of 51 patients who have normal aided scores on the same speech in noise test shown by Glick and Sharma to signal brain resource preservation in hopes of identifying those therapeutic steps that can properly reset the brain.
Those interested in obtaining further information on this topic are invited to the monthly meeting of the Oregon Association for Better Hearing at Corvallis Good Samaritan Hospital, Conference Room B on the second Thursday of every month from 3:30 to 5:00 p.m.
Click Here for the Upcoming Seminar Information
How the Aging Brain Affects Speech Understanding in Noisy Places
In recent years the focus on hearing health care has shifted from the ears to the brain. One needs to only Google hearing loss and cognition to find dozens of articles in medical and hearing health care journals in the past few years. [Read more…]
Divergent Views in Hearing Health Care
In August of 2017 the face of hearing health care changed with the passage of the Over-the-Counter Hearing Aid Law, allowing consumers to self-diagnose and self-treat their hearing loss.
The events leading up to this change were spearheaded by two distinct groups. One group was from Johns Hopkins Medical University; the other from Indiana University. [Read more…]
Can Hearing Aids Unscramble the Brain?
A recent publication from Dr. Anu Sharma and colleagues at University Colorado, Boulder showed people who achieve a normal score with their hearing aids on a difficult speech in noise test were spared the brain resource reallocation reported for her subjects who have untreated or poorly treated hearing loss, perhaps explaining the strong relationship between hearing loss and dementia as noted by Dr. Frank Lin and colleagues at Johns Hopkins. [Read more…]
The Impact of Untreated Hearing Loss
“Hearing loss is not a harmless condition to be ignored or left untreated. It has tremendous impact on your life, and if left untreated, it can have serious emotional, (cognitive) and social consequences.” (Dr. Serge Kochkin, 2005).
Many people are aware Corvallis has a consumer education group for people who are hard of hearing. This group has met monthly since September 1988 and brings the latest scientific information to the community regarding hearing loss and hearing aids. Meetings are free to the public and take place on the second Thursday of each month from 3:30 to 5 p.m. at Corvallis Good Samaritan Hospital. [Read more…]
Why Are Hearing Aids So Expensive?
Why Are Hearing Aids So Expensive?

As Founder of the 32-year-old Oregon Association for Better Hearing (OABH) this question has been posed dozens of times during our monthly meetings.
When you look at the literature concerning hearing aid expense, several explanations for the high cost of hearing aids are put forth. [Read more…]
Debate on Medicare &Hearing Healthcare
Several sources estimate Medicare will be insolvent by 2028. This dire prediction has produced numerous suggestions regarding how to cut medical costs and maintain Medicare.
In the area of hearing healthcare this charge for Medicare cost efficiency is led by otolaryngologist Frank Lin of Johns Hopkins Medical University.
Dr. Lin has suggested hearing healthcare could be more affordable by first removing all medical oversight for adults with mild-to-moderate hearing loss allowing them to self-diagnose and self-treat their hearing losses. [Read more…]